Strategies for Outsourced Revenue Cycle Management
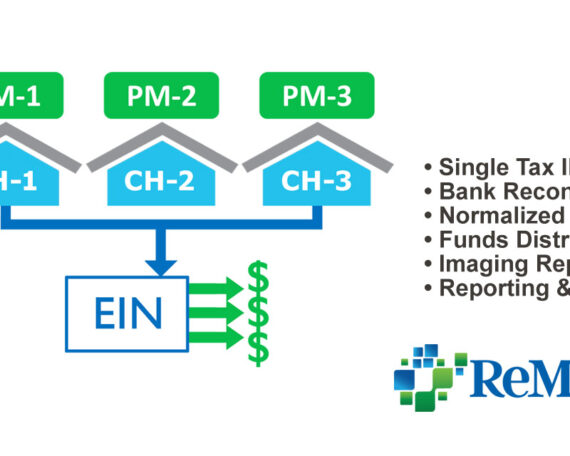
Strategies for Revenue Cycle Outsourcing in a Co-Shared Business Model For many healthcare provider organizations, staffing shortages continue to create a variety of cash flow obstacles. In researching different outsourcing options, solutions will range from a specific area of need to a substantial portion of your business office. In most cases, ReMedics provides a co-shared