Automating Revenue Cycle Processes
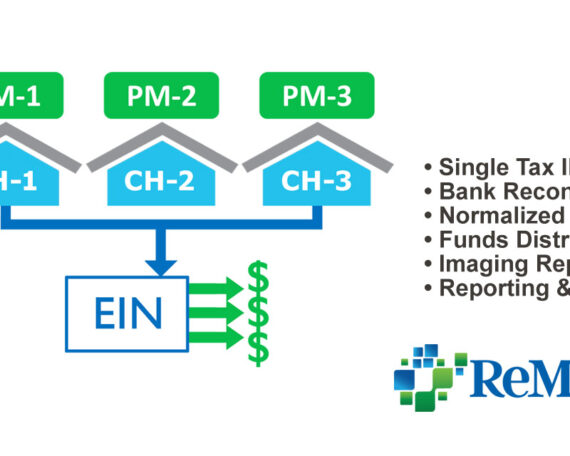
Streamlined Workflows for Improved Processing Speed and Data Accuracy Automating the Capture and Routing of All Payments and Correspondence In order to streamline remittance processing work with minimal errors, ReMedics enhances the data capture of all payments to include adjustments, zero pays and comments. Integrated to any major Practice Management (PM) System (or multiple systems)