Tailored Solutions for Optimizing Reimbursement and Cash Flow Improving Financial Performance – Integrated with Existing EMR/PM Systems Healthcare organizations lose millions each year in net revenue due to complicated reimbursement methodologies, regulatory issues, increasing patient payment responsibility, and growth in self pay or uninsured patients. Reallocating resources to improve financial
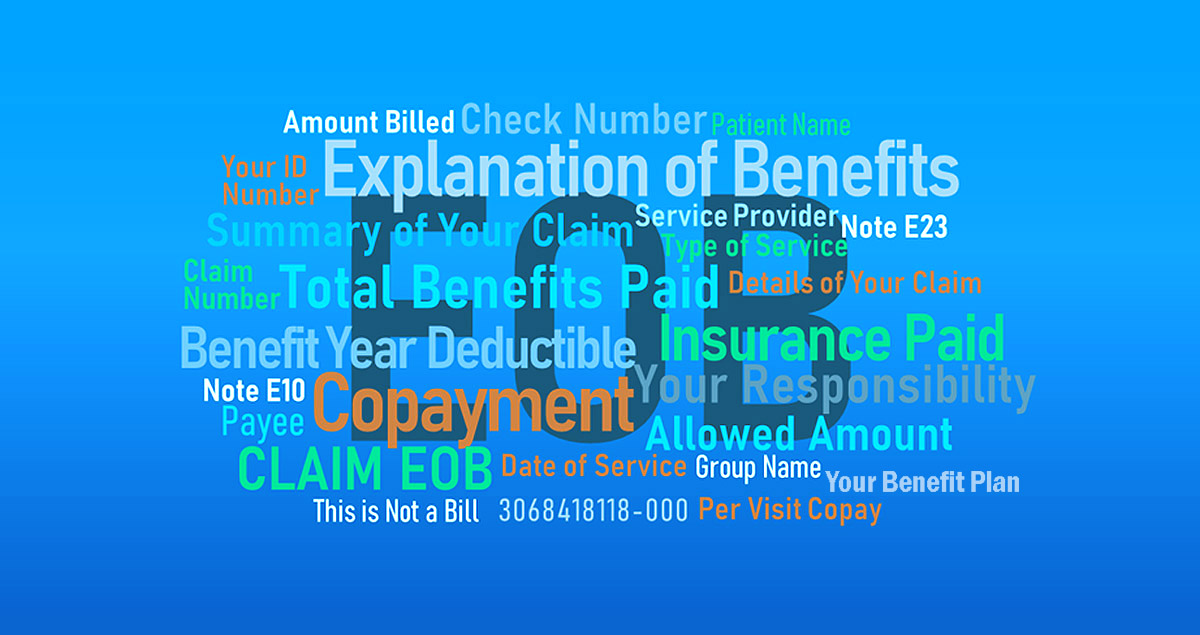
Capturing Your Paper EOB’s and Correspondence Document Capture, Indexing & Retrieval With the ReMedics Document Management Portal, accounting personnel can quickly search and retrieve EOB and correspondence files by Patient Last Name, Check Number, Invoice Date, Paid Amount and many other “wildcard” options to easily identify any missing information needed
Identifying and Re-Associating PLBs The following is an excerpt from our client support newsletter called “A Closer Look”, which provides helpful information in dealing with common payment processing, denial/defect and reconciliation issues. This particular article looked into the complexities associated with Provider Level Balance Adjustments (aka PLBs). If you would
Converting EOBs to 835 Electronic Remittance Advice Optical Character Recognition (OCR) in its simplest form is the process whereby a paper document is scanned and the image is captured for processing data into a specific application, such as paper-based EOBs. The text is extracted from an image and converted into
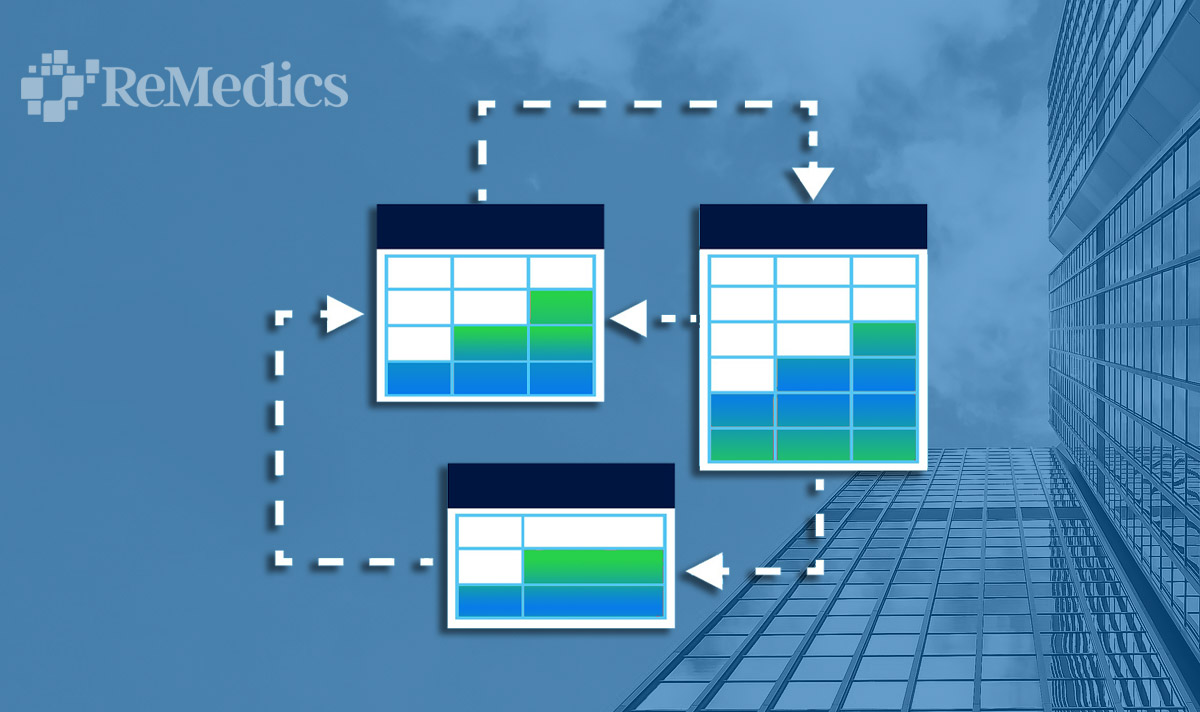
Using RPA in Revenue Cycle Applications Can RPA improve your revenue cycle? The quick answer is definitely yes, with the right technology and experienced systems integration partner. A subset of Artificial Intelligence (AI), ReMedics uses Robotics Process Automation (RPA) in our Operations Group to create streamlined workflows where the need
ReMedics and Your Bank Accounts The Process Behind the Processing Knowing how ReMedics interacts with our clients’ bank accounts is an important area of understanding the processing that takes place. For many of our clients, we work very closely with the bank associated with the “Corporate Lockbox” account. This is
Denial Prevention and Increased Staff Efficiency Benjamin Franklin is credited with having coined the phrase, “An ounce of prevention is worth a pound of cure.” It’s as relevant today as it was in 1736, especially when it comes to healthcare payor denials. In a recent survey* reported by Becker’s Healthcare,
Correspondence Management and Workflow Efficiency For healthcare provider organizations, unstructured content exists in a wide variety of file types and sources of information. Being able to quickly retrieve lockbox correspondence, indexed to the patient, can play a critical role in how fast your claims get paid, delayed or denied due
Maintaining Your Clearinghouse & Banking Relationships Our client’s Clearinghouses and Banks play an important role in how medical claims are submitted and how insurance payors provide reimbursement back to the physician group. Clearinghouse services go beyond just claim submission and remediation. Their services can also include eligibility and benefits checking,