
Denial Defects and Denial Management
Claim denials greatly impact the revenue cycle by delaying or reducing payments from payors to providers. While denials can cause a significant amount of revenue loss, most of them can be avoided.
Denials are simply the result of a rules-set, programmed within the payor system to look for matching information in a myriad of patient and contract databases. ReMedics ensures that the claim process is managed and audited to stop recurring denials — with reporting & analytics tools to help identify the root cause of problem areas.
While ReMedics goal is to prevent denials from occurring altogether, we provide our clients with the right workflow efficiency tools to quickly get them appealed and resolved.
Automated Data Validation and Workflow
Data validation is at the heart of ReMedics Denial Prevention. Validation helps to scrub and cleanse the data before posting. We automatically check for errors, validating all claim information needed for processing while improving data integrity. Once data is captured (EDI or paper), our payment validation process begins applying over 300 client customized rules to find potential cash application errors before posting and routing those errors back to work queues for correction.
Correspondence and Work Queue Follow-Up
Working in tandem with our proprietary Payment Processing technology, our Denial Management application captures denials in the system and then routes them for automated correspondence and work queue follow-up. By having a single source of denial information and correspondence, we create efficiency in your billing office and accountability for managing all denials.
Denial Analysis Scorecards
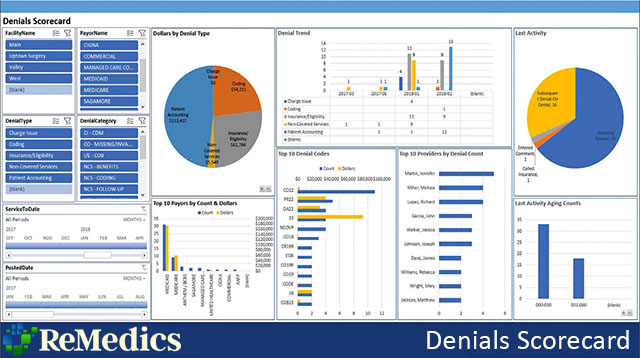
Denials trends can be analyzed and traced to specific areas, from patient access and eligibility to individual physicians, departments or type of service.
By providing a complete record of all denials, with Power BI drill-down capabilities, we provide valuable insight into where errors are more likely to occur in your claim and billing processes. By taking a proactive approach to Denial Management, cash flows are increased, and overall cost to collect is reduced.
Let’s talk about how we can help to reduce your initial denial rate altogether and help to make appeals more efficient for your organization. Contact ReMedics today to get started.
