
ReMedics Comprehensive Collection Services
For clients needing flexibility in managing their business office, ReMedics delivers comprehensive collection solutions that help to lower operational costs, increase staff productivity and maximize reimbursements. We bring extensive revenue cycle management experience in creating workflow solutions that increase efficiency, improve data quality and optimize A/R performance. Our technology allows us to collaborate with your team in a co-shared environment to increase cash collections, decrease errors and reduce your aged receivables.
Utilizing the RCMS ReSolve® A/R Management Platform, ReMedics can integrate to multiple EMR/PM systems, banks and clearinghouses. With the use of robotics process automation and artificial intelligence, we leverage our client’s existing IT investments to produce cost-effective departmental work processes, robust data validation, reduced denial defects and dynamic reporting.
Denials & Customized Follow Up Activity
Utilizing our system, we can provide a more robust data set to the client and/or the ReMedics operations team to focus on claims in many custom formats, including categorization for complex denials to ensure they are being systemically worked for processing. We specialize in revenue cycle optimization to prevent reimbursement delays and claim denials with the use of automation and provider/staff education.
ReMedics offers customized follow up activity based upon the type of denial, by payer, aging, dollar value and other criteria. Let us know your specific requirements for a customizable plan that provides the best return on investment for your organization.
Our Comprehensive Services
- Work all billing related edits in the clearinghouse
- Work all clearinghouse and payer rejections
- Provide a review of all accounts as required
- Initiate work on denials from insurance companies within 48 hours of receipt
- Provide telephone access for insurance company inquiries regarding billing and collection issues
- Initiate work on Government payers at day 15 and Commercial payers at day 30 from claim submission date
- Analyze and work all short pays based on contracted rate
- Analyze all overpayments for validity
- Review and work all recoups from the payer
- Provide scheduled updates to reports and scorecards on all billed revenue and work processes
- Provide staff with ReMedics web-based document imaging portal for access to all captured and indexed correspondence
- Customer support, training, and professional services as needed.
Reporting & Analytics
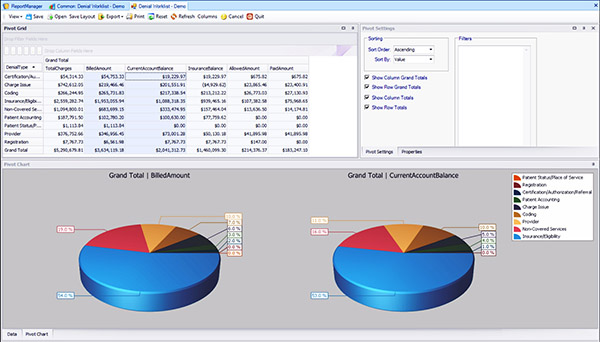
ReMedics reporting includes pivot charts and scorecards that help to quickly identify hidden trends.
We provide our clients with robust reporting options to review details on all claim submissions, payments, denial/defects and collection activities. Our integration capabilities with clearinghouse(s), line of business applications, and banking partners deliver an analytical view of billed revenue and denials by business unit, physician, specialty, procedure or payer.
Correspondence Document Management
ReMedics has the ability to index and categorize all correspondence from the client’s lockbox for more efficient, timely follow-up on appeals and collections. We can also provide our clients with web-based access to their correspondence documents through OnBase, the industry-leading enterprise content management solution from Hyland Software.
Talk to ReMedics
Let us know if you would like more information about our Comprehensive Collections Services. For hospitals and physician practice groups, we can also provide streamlined remittance processing, data validation and bank reconciliation for organizations using several EMR/PM vendors and EDI clearinghouses. Talk to us about your specific outsourcing needs to see how we can help.

